6 ICHRA Compliance Requirements Employers Should Know for 2024

What are the compliance and reporting requirements of ICHRA?
ICHRA is a tax construct; anytime the government is involved, you can expect paperwork. These are the tax forms that you need to know:
1095-A
Form 1095-A refers to the Health Insurance Marketplace Statement. If your employees obtained coverage from Healthcare.gov or a state-based exchange (e.g., CoveredCA, Washington Health Finder, MNsure, etc), they will receive a 1095-A. Healthcare.gov and the state-based exchanges send it out.
What is the 1095-A? This form is used to reconcile Advanced Premium Tax Credits (individuals receiving premium subsidies from the government) or claim the Premium Tax Credit.
Here’s the catch: any employee participating in any group health insurance plan (including an ICHRA) is not eligible for the Advanced Premium Tax Credit or the Premium Tax Credit. Form 1095-A primarily applies to self-employed individuals or individuals who do not receive employer-sponsored benefits.
Even still, many employees participating in an ICHRA will receive a 1095-A in early January. The Form 1095-A typically says “$0.00” since they did not receive premium tax credits.
What do employees need to do? Employees can submit this form as part of their tax returns. Employees should consult a tax professional should they need additional guidance.
What do employers need to do? Direct employees to Venteur for assistance as needed.
1095-B
Does the phrase “individual mandate” ring a bell? When the Affordable Care Act (ACA) was first passed, the new law required everyone to have health insurance or face a tax penalty (aka, the “Individual Mandate.”)
What is the Form 1095-B? Form 1095-B serves as proof of Minimum Essential Coverage. It is the IRS’s way of checking that you met the “Individual Mandate” or whether you’re required to pay fines. Health insurance carriers provide the Form 1095-C directly to individuals.
Here’s the catch: The Federal Government eliminated the “Individual Mandate” requirement at the end of 2018. Right about now, you might be thinking, “OK. Then what’s the point of the Form 1095-B.” You have a point. Some insurers no longer send out 1095-B forms and will only provide them upon request.
Still, some states continue to have “Individual Mandate” requirements. These include California, the District of Columbia, Massachussetts, New Jersey, Rhode Island, and Vermont. Form 1095-B certifies that the individual has met these jurisdictions' “Individual Mandate” requirements.
What do employees need to do? Form 1095-B is typically submitted as part of an individual's tax return -- especially if you live in a state with “Individual Mandate” requirements. Employees should consult a tax professional should they need additional guidance.
What do employers need to do? Direct employees to Venteur for assistance as needed.
1094-C and 1095-C
The Affordable Care Act requires all employers with 50 or more full-time equivalent employees (FTEs) to provide health insurance to their workforce. Form 1094-C and 1095-C are annual tax filings required of Applicable Large Employers (ALEs) confirming that they have met their obligations under the law (aka, “the Employer Mandate.”) ICHRAs allow employers to satisfy these ACA requirements.
What is Form 1094-C? Form 1094-C is an annual filing that employers must make to the IRS detailing their employer-provided health insurance offer and coverage. The IRS uses this form to determine whether employers have met ACA requirements or whether to assess penalties.
What is Form 1095-C? Form 1095-C is an annual IRS filing that employers must provide to employees detailing their employer-provided health insurance offer and coverage.
What do employees need to do? Form 1095-C is typically submitted as part of an individual's tax return. Employees should consult a tax professional should they need additional guidance.
What do employers need to do? File the 1094-C and 1095-C with the IRS by February 28th (for paper filings) or March 31st (for digital filings). Distribute the 1095-C to employees in advance of the deadlines. Venteur helps prepare the data employers need to make these filings.
** NOTE: Only Applicable Large Employers (employers with 50 or more full-time equivalent employees) must file the 1094-C and 1095-C. Small businesses do not have to file a 1094-C or 1095-C.
Patient-Centered Outcome Research Institute (PCORI) Fees
Employers who offered an ICHRA or self-funded plan in 2023 must pay a PCORI fee. It is due by July 31st, 2024.
What is the PCORI fee? The federal government imposes an annual fee to help fund the Patient-Centered Outcomes Research Institute, a non-profit research institute that supports research on clinical effectiveness. The current PCORI fee is $3 per covered individual.
What do employees need to do? No action is required.
What do employers need to do? Use Form 720, Quarterly Excise Tax Return, to file your PCORI Fee and pay the IRS by the July 31 deadline. Venteur will provide employers with data to prepare their filing and instructions on how to do so.
Form 5500
Any employer offering benefits to their employees is acting as a fiduciary. The Employee Retirement Income Security Act (ERISA) sets rules to protect the rights and interests of employees and their beneficiaries. Form 5500 is a mandatory Annual Report designed to ensure ERISA.
What is the Form 5500?
Filed with the U.S. Department of Labor and IRS, [Form 5500] (https://www.dol.gov/agencies/ebsa/employers-and-advisers/plan-administration-and-compliance/reporting-and-filing/form-5500)discloses comprehensive information about an employer’s benefit plan. Employers must file Form 5500 for each benefit they sponsor, including ICHRAs.
What do employees need to do?
No action is required.
What do employers need to do?
File Form 5500 by the seventh month after the plan year ends. For most employers, this deadline is July 31st. Venteur will assist employers with preparing the data inputs and preparing instructions on how to file Form 5500.
COBRA
Consolidated Omnibus Budget Reconciliation Act (COBRA) allows departing employees to keep their health plan even after they have left their jobs. Employers with 20 or more employees in the prior year must offer COBRA.
COBRA and ICHRA? COBRA under an ICHRA works a bit differently. Employees are the policy owners of their health insurance plans. If they want to keep their plan, all they need to do is take over premium payments. To learn more, read our COBRA overview article.
What do employees need to do? Decide whether they want to:
- Keep their health insurance plan and take over premium payments
- Cancel their health insurance plan
- Opt into COBRA
What do employers need to do? Coordinate with Venteur to let us know of departing employees. We’ll send out COBRA notices (or provide you with templates to send out).
Compliance Made Easy
At Venteur, we strive to make compliance easy for employers and employees. We understand the importance of adhering to regulations and ensuring your employees have the necessary information and support. Whether it's handling tax forms like 1095-A, 1095-B, 1094-C, and 1095-C, or managing requirements like PCORI fees and COBRA, we're here to assist you every step of the way. Please don’t hesitate to get in touch if there’s a question we can answer for you.
You got questions, we got answers!
We're here to help you make informed decisions on health insurance for you and your family. Check out our FAQs or contact us if you have any additional questions.
Explore more related content
What is Venteur
Explore the best human-first Health Insurance platform
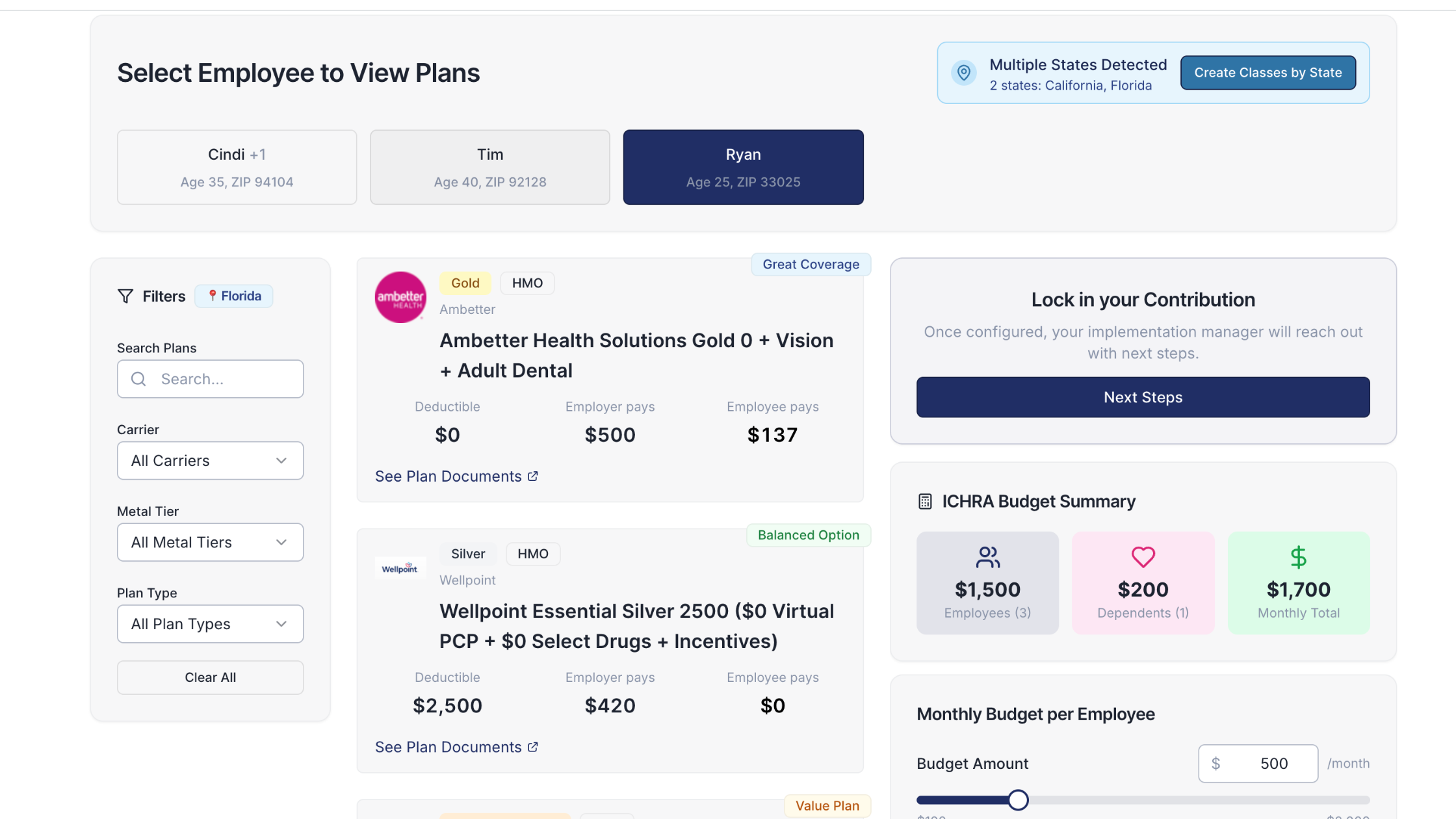
Simple, personalized health benefits
Sign up in minutes, define your contribution, and let your employees choose the health plan that works right for them
Integrations to make everything run smoothly
We'll connect with your payroll and finance systems to make deductions and premium payments seamless
Easy onboarding and off-boarding
In just a few clicks, add your roster and make updates on the fly. We'll handle it from there.
Venteur Certified Brokers to help your employees pick the right plan
Our trusted brokers ensure the best outcomes for employees and employers by unlocking health savings and providing unrivaled plan options.
AI-powered plan recommendations to give you confidence while you shop
Backed by 30 years of healthcare data, Venteur’s AI helps employees compare and choose the best plan for their unique situation.
Compliance and reporting because no-duh!
Venteur manages plan administration, reporting, and compliance so you can focus on growing your business.